The impacts of the pandemic can be seen in all aspects of society. As most individuals focus on the advice of public health officials on COVID-19, many other concerns lack the attention they deserve. Most notably, many health officials are increasingly concerned about the long-term risks that will result from individuals delaying non-urgent medical procedures, many of which are being postponed due to fears of going into a medical practice.
According the Health Care Cost Institute (HCCI), the “pandemic has…brought a set of (seemingly endless) new trade-offs and choices for people to make as they navigate their daily lives, and the health care system. Among them, whether, when, and how to resume their pre-pandemic health care life.” The HCCI, to evaluate the impact of health care consumption as a result of COVID-19, looked at a sample of health claims clearinghouse records from 18 states containing 184 million claims from 30 million patients in 2019 and 94 million claims from 20 million patients for the first six months in 2020. The analysis found that the pandemic significantly reduced the consumption of preventive health care. The chart below compares use of the select services between 2020 and 2019 using a 7-day rolling average.
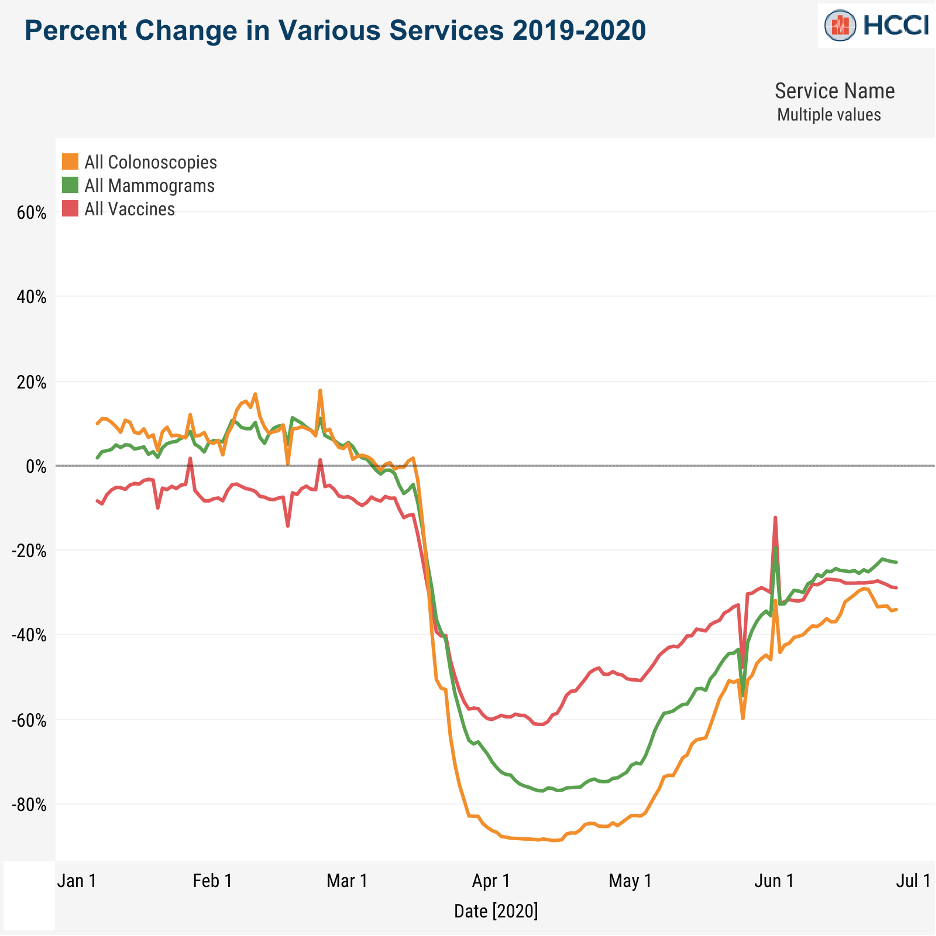
The HCCI offered detailed analysis of a number of procedures, but chart above highlights the general trend. That is, non-urgent health care services dropped precipitously early in the pandemic. This was the result of medical offices closing or dramatically scaling back as well as concerns from patients about contracting the virus while visiting a health care facility. Although there was been a steady recovery in claims through May and June of 2020, utilization of health care remains substantially low.
The thing that jumped out at me was how similar all the patterns were. The bottom was deeper for some services than others, but the slope of the lines was pretty similar no matter what service you picked.
– Niall Brennan, HCCI President
Public Health Concern
As medical offices opened and shutdowns subsided, many experts felt that health care would see a surge in demand as patients made up for deferred care. Early data suggests that may not be the case. Although, it is important to note that the data from HCCI ends in June of 2020, and due to lags in claims processing, June numbers could inch upwards.
Health officials are concerned that if the vast majority of deferred health care does not come back, there may be some serious public health ramifications. For example, the anti-vaccination movement was already increasing the rate of measles in the US prior to the pandemic. Since the pandemic, measles vaccinations fell 73% in mid-April and were still down 36% at the end of June. With less children vaccinated, especially if they do not get vaccinated later, there are fears that measle outbreaks may continue to trend upward, putting unnecessary costs onto the health care system.
Health care researchers believe it will take years to discover the long-term impact of deferred preventive procedures. Will fewer colonoscopies, for example, translate into more cases of advanced colon cancer? Will there be more outbreaks of communicable diseases because of lower vaccination rates?
Employers Need To Educate
Since many of these long-term costs will impact companies that provide health insurance to their employees, it is in their best interest to educate, facilitate, and remind employees about the importance of certain preventive health care services. The best place to start is by promoting all employees to get a flu shot this season.